How Should They be Treated? What is Orthopaedic Prosthesis Infection?
Orthopaedic infections constitute of a significant problem due to increased number of hip and knee arthroplasties around the world. While artificial joints can increase a patient’s life quality significantly, prosthesis insufficiency and infection can cause high disease ratio and pain.
How do Orthopaedic Prosthesis Infections Occur?
When periprosthetic infections are considered, there are two main path and time scale regarding bacteria penetration. The first is the perioperative period where the source is the endogeneous bacteria or microorganism around the hospital personnel or surgical room; the second is hematogeneous spread which occurs during post-operative period. The placement of prosthesis in the human body increases the risk of infection that can mature in biofilm. Since orthopaedic infection problems can continue in the years following orthopaedic surgery in acute patients or chronic, infection diagnosis is still a challenging work for health specialists.
Treatment of Orthopaedic Prosthesis Infections
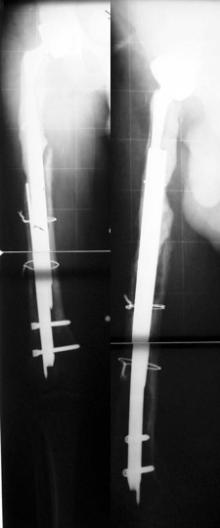
Osteomyelite is a devastating disease of bone tissue and is a serious complication in orthopaedic and trauma surgery especially when prosthesis and osteosynthesis are used together. The infection risk of a prosthesis/osteosynthesis is related to the location of implant and health condition of the patient. While hip and knee prosthesis have risk of infection up to 1-5%, osteosynthesis with the purpose of trauma surgery has higher infection risk ratio. When the increasing number of implants and fixed infection ratio of these implants are considered, it means that this will cause prevalence of implant infections to increase. Alongside this, infection treatment is usually based on local antibiotics treatment combined with surgery. Generally, it is observed that a revision with two stages which has 93% success rate is the most efficient infection treatment. On the other hand, infection prevention is based on preventing or delaying bacterial adhesion on the implant surface and eukaryotic cells surviving and finding a more suitable surface to adhere to.
Treatment of orthopaedic prosthesis infections is usually applied in two stages. In the first stage, existing prosthesis in hip or knee is removed with minimal damage by specialists and with proper methods. Then the infected tissue is removed. Therefore healthy and bleeding bone and soft tissue is reached. Then the region is cleaned with the help of serum physiologic. The prepare the patient for the surgery again, the disinfection process is repeated and the patient changed into a new surgical dress and a new cover set is used. The second stage of the surgery is started. In the second stage, a temporary prosthesis with antibiotics called spacer that will take the place of the joint in hip or knee and protect it is placed. Suitable antibiotics are placed in this spacer. Therefore, it is allowed to treat the infection region more closely with antibiotics. Alongside this, suitable antibiotics produced with culture samples taken during the surgery are given to the patient through the veins for 4-6 weeks. For about this much duration, the patient is taken into the period without antibiotics. At the end of nearly 3 months, if it is determined the infection is treated with blood tests if necessary (Leukocyte, CRP and ESR count), the second stage of the treatment is started. In the second stage, the placed temporary implant is taken out and after wound cleaning and washing, the patient is prepared for the surgery again with new cover sets. Prosthesis with suitable dimension that is prepared for the bones prepared with proper cuts is fixed with the help of cement (for knee prosthesis) with antibiotics. Hip prosthesis can also be placed without using cement if femoral channel and acetabulum is prepared enough. Monitoring after the surgery is performed not only with roentgen, but also with laboratory tests once every 3 months. The success rate of these treatments (cleaning of infection) demonstrates the importance of using local antibiotics in implant infection treatment.